Cauterization of the uterus is a medical procedure used to treat abnormal uterine bleeding, control hemorrhage, or remove abnormal tissue from the uterine lining. This procedure is often considered when conservative treatments such as medication or hormone therapy have not been effective. Uterine cauterization can involve various techniques, including thermal, electrical, or chemical methods, depending on the patient’s condition, medical history, and the healthcare provider’s expertise. Understanding the procedure, indications, preparation, and potential risks helps patients make informed decisions and ensures safer outcomes.
Indications for Uterine Cauterization
Uterine cauterization is primarily indicated for women experiencing abnormal uterine bleeding that does not respond to medication. Conditions such as heavy menstrual bleeding, postmenopausal bleeding, fibroids, or polyps may warrant this procedure. It is also used in cases where there is a need to remove abnormal endometrial tissue that could potentially lead to precancerous changes. In some situations, cauterization is employed to control acute uterine hemorrhage following childbirth or surgical interventions.
Types of Uterine Cauterization
The procedure can be performed using different techniques, each with specific advantages and considerations
- Thermal Cauterization Uses heat energy to burn or destroy abnormal tissue within the uterine lining.
- Electrocautery Employs electric current to achieve tissue destruction and control bleeding.
- Chemical Cauterization Involves the application of chemical agents to induce tissue coagulation and reduce bleeding.
Pre-Procedure Preparation
Before undergoing uterine cauterization, patients typically undergo a thorough evaluation, including a physical examination, medical history review, and diagnostic tests such as ultrasound or hysteroscopy. Blood tests may be conducted to assess hemoglobin levels and overall health. Patients are advised to avoid certain medications, such as blood thinners, prior to the procedure to minimize the risk of excessive bleeding. Fasting may be required if general anesthesia is planned.
Informed Consent
Obtaining informed consent is a critical step before the procedure. Patients are educated about the goals of cauterization, expected outcomes, potential risks, and alternative treatments. This discussion ensures that patients understand the procedure and can make informed decisions regarding their care.
The Procedure
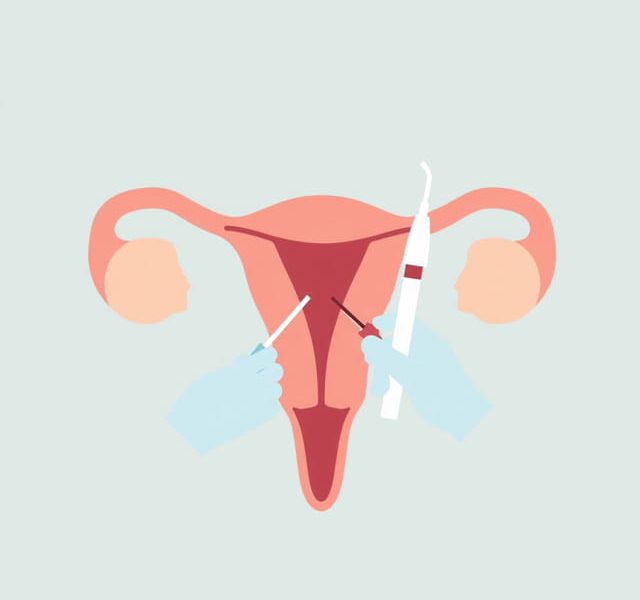
Uterine cauterization is typically performed under local, regional, or general anesthesia, depending on the patient’s condition and the technique used. The patient is positioned to allow access to the uterus, and the cervix may be dilated to permit entry of the cauterization instrument. The procedure involves precise application of heat, electric current, or chemical agents to the targeted areas of the uterine lining.
Steps in the Procedure
- Patient preparation and anesthesia administration to ensure comfort and safety.
- Dilation of the cervix, if necessary, to allow the insertion of the cauterization device.
- Insertion of the cauterization instrument, such as a thermal probe or electrocautery device, into the uterine cavity.
- Careful application of energy or chemical agents to the abnormal tissue while monitoring the patient’s response.
- Removal of the instrument and assessment of the uterus to ensure adequate treatment of the targeted area.
- Post-procedure monitoring to observe for bleeding, infection, or other complications.
Post-Procedure Care
After uterine cauterization, patients are monitored for a short period to ensure stability and proper recovery. Mild cramping, light bleeding, or discharge may occur for several days following the procedure. Healthcare providers often prescribe pain relief medications and may recommend avoiding sexual intercourse, tampons, or strenuous activity for a short period to promote healing. Follow-up appointments are essential to assess the effectiveness of the cauterization and monitor for potential complications.
Potential Risks and Complications
Although uterine cauterization is generally safe, potential risks include infection, excessive bleeding, damage to surrounding tissues, or scarring of the uterine lining. In rare cases, the procedure may affect future fertility or increase the risk of uterine perforation. Patients should promptly report severe pain, heavy bleeding, fever, or unusual discharge to their healthcare provider. Proper technique, adherence to sterile procedures, and careful patient selection significantly reduce the risk of complications.
Benefits of Uterine Cauterization
The primary benefit of uterine cauterization is the reduction or elimination of abnormal uterine bleeding, which can significantly improve a patient’s quality of life. By targeting the abnormal tissue directly, the procedure offers an effective and minimally invasive alternative to more extensive surgical interventions such as hysterectomy. It can also be used as a therapeutic tool for managing precancerous lesions or controlling acute hemorrhage, providing both immediate and long-term benefits.
Effectiveness and Outcomes
Clinical studies suggest that uterine cauterization is effective in controlling abnormal bleeding for a significant proportion of patients. Long-term outcomes depend on the underlying condition, the extent of abnormal tissue, and patient-specific factors such as age and reproductive goals. Regular follow-up and monitoring are essential to ensure sustained benefits and address any recurrence of symptoms.
Considerations for Fertility
For patients who wish to maintain fertility, careful consideration is required before performing uterine cauterization. Techniques are chosen to minimize damage to the healthy endometrial tissue. In some cases, alternative treatments may be recommended if preservation of fertility is a priority. Patients planning future pregnancies should discuss potential implications and options with their healthcare provider.
Alternative Treatments
In addition to cauterization, several alternative treatments exist for abnormal uterine bleeding or abnormal tissue within the uterus
- Medications such as hormonal therapy or nonsteroidal anti-inflammatory drugs to control bleeding.
- Minimally invasive surgical procedures like hysteroscopic polypectomy or endometrial ablation.
- Lifestyle modifications and management of underlying conditions contributing to abnormal bleeding.
The choice of treatment depends on the patient’s medical history, severity of symptoms, age, and reproductive goals.
Uterine cauterization is a valuable procedure for managing abnormal uterine bleeding, controlling hemorrhage, and treating abnormal tissue within the uterus. With proper patient selection, careful technique, and post-procedure care, the procedure can effectively reduce symptoms and improve quality of life. Patients should be informed about the indications, procedure steps, potential risks, and alternative treatments to make well-informed healthcare decisions. Regular follow-up ensures monitoring of recovery and assessment of long-term outcomes, making uterine cauterization a safe and effective option for women requiring intervention for uterine abnormalities.
Overall, understanding the procedure to cauterize the uterus, along with its benefits, risks, and post-operative care, empowers patients to actively participate in their treatment planning and achieve optimal results while minimizing complications.